DIEP Flap vs. Implant Breast Reconstruction
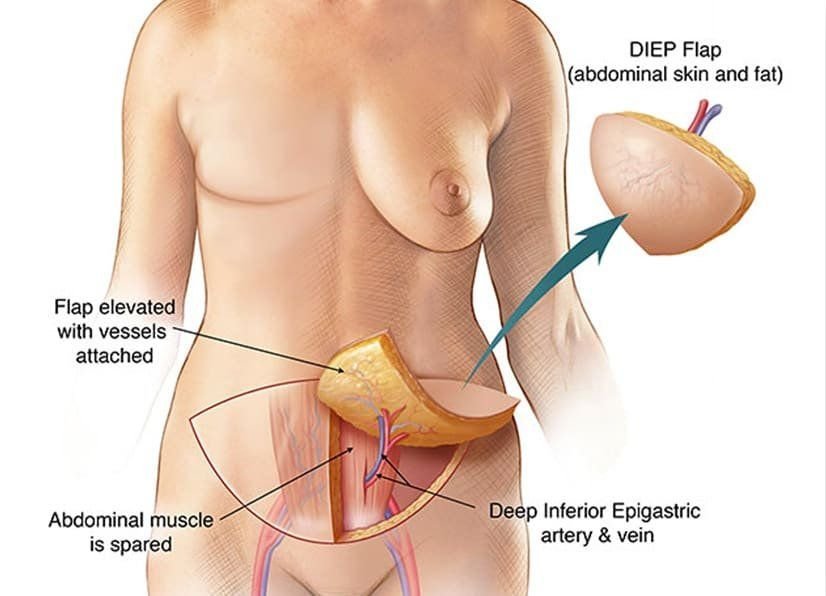
Breast cancer patients now have a lot of options when it comes to reconstructive surgery. The Deep Inferior Epigastric Perforator flap, also known as DIEP flap, replaces the soft tissue and skin removed during mastectomy with abdominal tissues[sup](1)[/sup]. This is an advanced method of breast reconstruction; unlike the TRAM flap procedure, the DIEP flap preserves all the muscles of the abdomen.
The procedure is available at Breast Reconstruction Associates, your DIEP flap providers in Dallas Fort Worth, Texas. Our goal is simple: we offer a state-of-the-art breast reconstruction option to women through a team approach of individualized and compassionate care.
The benefits of the DIEP flap vs. implant breast reconstruction are as follows:
1. The patient’s skin and fat are utilized to replace the breast volume that is removed during the mastectomy. This avoids the need to use an implant to recreate the breast volume.
2. Implant reconstruction patients may experience implant ruptures or capsular contracture, also known as breast hardening, that may need one or more maintenance surgeries years after their initial reconstruction. With DIEP flap reconstruction, the reconstructed breast tends to get softer and even more natural-feeling over time. After completing the DIEP flap reconstructive process, there is no anticipated maintenance necessary for the longevity of the reconstruction.
3. One advance in DIEP flap reconstruction is sensory nerve reconstruction of the flap. The hope with this additional step in a DIEP flap reconstruction is to provide sensation to the transplanted tissue. At this time, we are not doing this routinely in all cases, but rather it is offered in select patient scenarios. Your surgeon can discuss this option, review the pros and cons, and determine if sensory nerve reconstruction should be included as part of your reconstruction.
4. Post-operative pain is a common concern for patients considering DIEP flap reconstruction. It is often falsely assumed that implant reconstruction is less painful since it has a shorter operative time compared to the DIEP flap and does not involve surgery to the abdomen. At Breast Reconstruction Associates, we utilize a post-operative pain protocol that effectively manages most patient’s pain without requiring the use of narcotic pain medication.
In our practice’s experience, patient’s recovery and healing after DIEP flap reconstruction are actually significantly easier than what most people anticipate. Many of our patients choose to go home after a two-night stay in the hospital.
Truly, the DIEP flap is an excellent breast reconstruction option for women which results in a natural-looking and feeling breast after mastectomy, especially in women who prefer to avoid the use of implants. If you want more information about today’s “gold standard” in breast reconstruction, feel free to contact us at Breast Reconstruction Associates, your DIEP flap experts in Dallas Fort Worth, Texas.
Sources: