A Season of Renewal: Starting the New Year with Confidence After Breast Reconstruction
The holiday season is a time for reflection, gratitude, and hope. For women who have faced breast cancer, this time of year often carries a deeper meaning, a chance to celebrate survival, healing, and new beginnings. For many, this includes finding renewed confidence through breast reconstruction after mastectomy. At Breast Reconstruction Associates, we believe every woman deserves to enter the new year feeling whole, confident, and supported.
Whether you have completed your breast reconstruction or are considering it for the year ahead, December is the perfect time to focus on self-care, renewal, and embracing your next chapter with strength and confidence.
Reflecting on the Journey After Breast Cancer
The path through breast cancer treatment and recovery can be long and emotional. It takes incredible courage to face surgery, chemotherapy, or radiation. Many women describe the process as transformative, an experience that changes how they see themselves and what matters most in life. Many women also explore breast reconstruction after mastectomy as part of this healing process.
At Breast Reconstruction Associates, our team understands that breast reconstruction is not simply a surgical procedure. It is a personal and emotional part of your healing journey. We are honored to help women rebuild not only their bodies, but also their confidence and sense of self as they move forward after breast cancer.
Choosing Reconstruction After Mastectomy: A Gift of Confidence and Healing
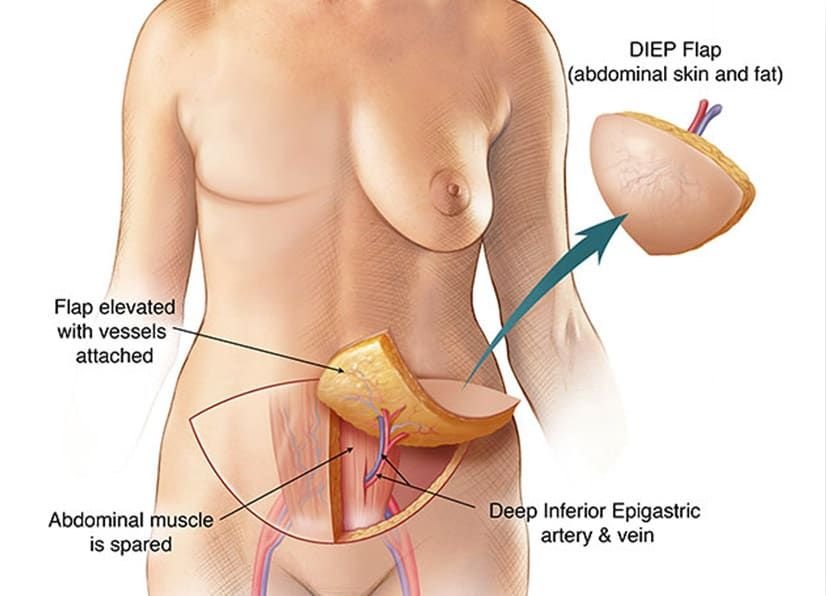
For women considering breast reconstruction after mastectomy, the decision to undergo surgery can feel empowering, a way to reclaim control and restore balance after cancer. Our surgeons specialize exclusively in advanced microsurgical breast reconstruction, including the DIEP flap procedure, which uses your own natural tissue to create soft, natural-looking breasts without sacrificing abdominal muscles.
Other options, such as PAP flap, GAP flap, and implant-based reconstruction, are available to meet every woman’s unique needs. Our approach is always personalized, ensuring that your care plan supports both your physical recovery and emotional well-being.
Healing with Support and Compassion
The holidays can bring complex emotions, joy, gratitude, and sometimes reflection on the challenges of the past year. If you are navigating breast cancer recovery, know that you are not alone. The team at Breast Reconstruction Associates provides compassionate, patient-centered care in a warm and supportive environment. If you are exploring breast reconstruction after mastectomy, we are here to guide you with compassion and clarity.
From your first consultation through recovery, we are here to answer your questions, ease your worries, and guide you through each step of your reconstruction journey. Our goal is to help you feel confident and empowered as you begin a new chapter in your life.
Looking Ahead: Hope and Confidence for the New Year
As the year comes to a close, take time to honor how far you have come. Healing after breast cancer is not just about physical recovery, it is about rediscovering your strength and celebrating your resilience.
If you are considering breast reconstruction in Texas, make 2026 the year you focus on yourself. Let Breast Reconstruction Associates help you move forward with renewed confidence, restored balance, and hope for the future.
Start Your Reconstruction Journey in the New Year
Your journey toward healing and wholeness begins with understanding your options. Our compassionate, board-certified surgeons specialize in DIEP flap surgery and other advanced techniques that deliver natural, lasting results.
Call Breast Reconstruction Associates today at 682-200-8580 or visit txdiepflap.com to schedule your consultation.
Let this new year mark the beginning of your renewed confidence, peace, and self-love.