Microsurgical Breast Reconstruction — Brought to You, Wherever You Are
At Breast Reconstruction Associates, we believe that every woman deserves access to the most advanced, compassionate breast reconstruction care, regardless of where she lives. That is why all of our surgeons are highly trained microsurgeons who travel to our clinics in various states to deliver this life-changing service directly to patients.
You should not have to sacrifice quality, safety, or expertise just because of your location. With Breast Reconstruction Associates, you do not have to.
What Is Microsurgery—and Why Does It Matter in Breast Reconstruction?
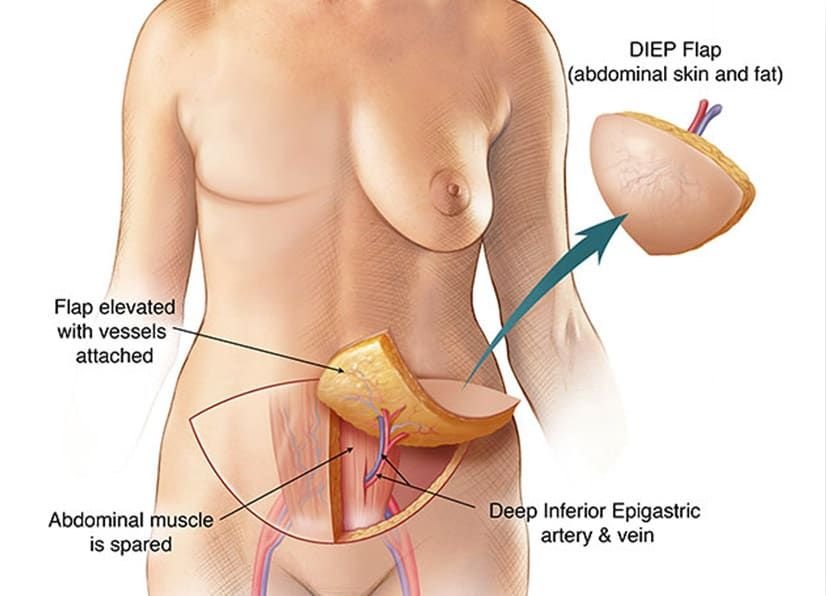
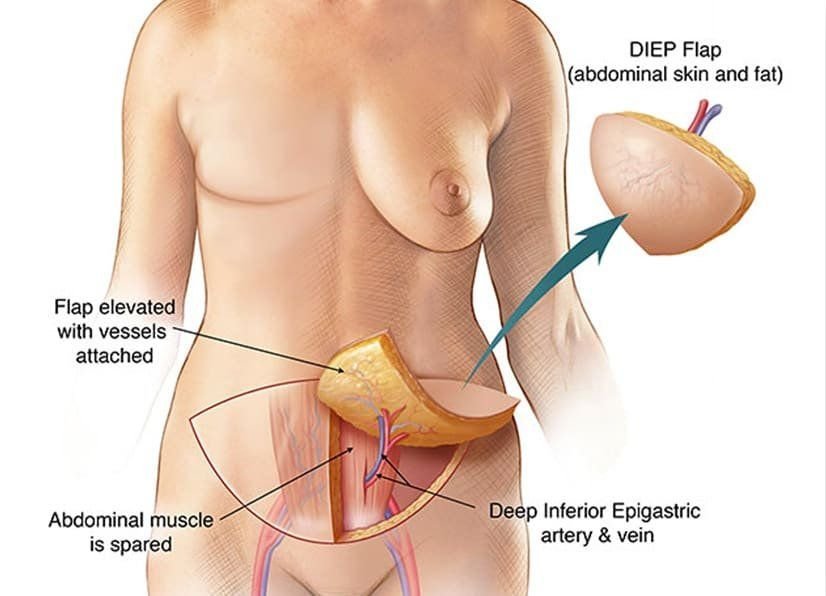
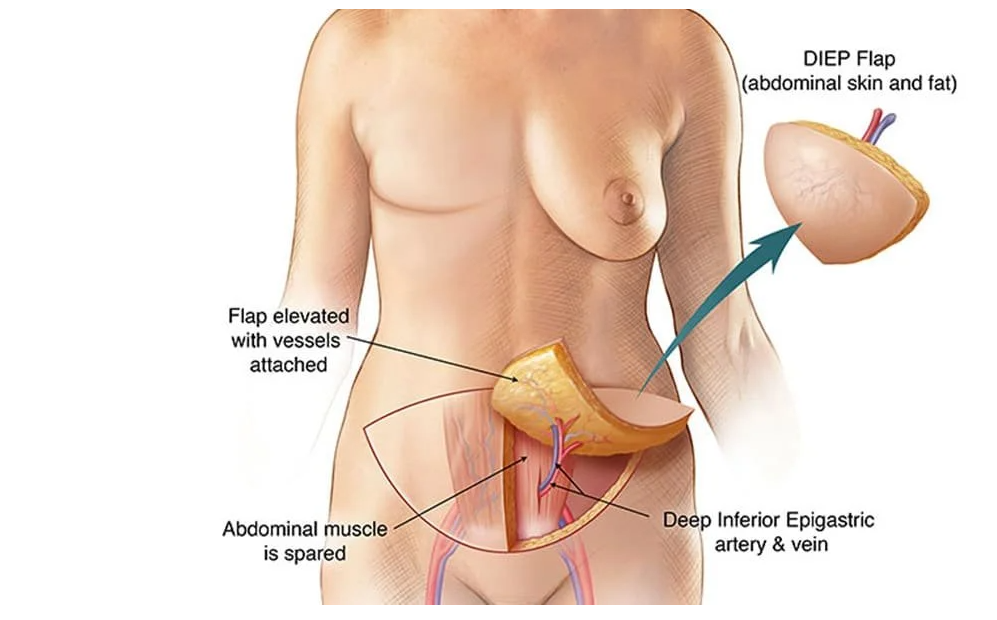
Microsurgery is a highly specialized surgical technique that involves reconnecting tiny blood vessels under a microscope. In breast reconstruction, it is most commonly used in DIEP flap and other natural tissue flap procedures, where the surgeon transfers living tissue from one part of the body (such as the abdomen, thigh, or buttocks) to recreate a soft, natural-looking breast.
This type of surgery requires advanced training, precision, and experience. It also allows for:
- Preservation of your abdominal muscles
- Shorter recovery times
- More natural results without implants
- Long-term durability and fewer complications
Microsurgical reconstruction is considered the gold standard for women who want a more natural reconstruction after mastectomy.
Our Surgeons Travel to Serve You
Unlike many practices, our team of board-certified plastic surgeons are all fellowship-trained in microsurgery. To make this high level of care accessible, they travel regularly to our partner hospitals and clinics in multiple states. This allows patients to receive world-class surgical outcomes in their own communities or close to home, without the burden of navigating care on their own.
Whether you live in Texas or another region, our traveling model ensures:
- You get treated by a surgeon who performs a high volume of advanced breast reconstruction cases
- You are cared for by a team that specializes exclusively in post-mastectomy reconstruction
- You experience continuity of care throughout your healing journey
Why Patients Nationwide Choose Breast Reconstruction Associates
We understand how overwhelming the choices can feel after a breast cancer diagnosis or mastectomy. Many patients come to us after being told they are not candidates for reconstruction, or after struggling with unsatisfactory results from prior surgeries.
Our team provides:
- DIEP flap and other muscle-sparing flap procedures
- Revisions of failed or painful implant reconstructions
- Reconstruction after radiation or delayed timing
- Individualized care from start to finish
We are proud to bring our expertise directly to you, whether you are in Dallas, Fort Worth, or another partner location across the U.S.
You Deserve National-Level Expertise—Close to Home
Healing after breast cancer is a deeply personal journey. Choosing the right reconstruction option can restore not just your body, but your sense of self. Our surgeons are honored to help women all over the country access the most advanced care in the most compassionate way.
Wherever you are—we are coming to you.
📞 Call us today at 682-200-8580 to schedule a consultation
🌐 Visit us at www.TxDiepFlap.com to learn more
📍 Serving patients in Texas and multiple partner locations across the U.S.