Gratitude After Breast Cancer: Finding Healing and Confidence Through Breast Reconstruction
As November arrives and the season of gratitude begins, many women reflect on the strength it takes to face and overcome breast cancer. For survivors, choosing breast reconstruction after mastectomy can be a deeply meaningful step toward physical and emotional healing. At Breast Reconstruction Associates, our caring team of breast reconstruction specialists is dedicated to helping women restore confidence and feel whole again.
Healing Beyond the Physical: The Emotional Impact of Breast Cancer
A breast cancer diagnosis affects every aspect of life—physically, emotionally, and mentally. After a mastectomy, many women experience feelings of loss, uncertainty, or changes in body image. These emotions are completely normal. Healing after breast cancer involves both the mind and the body, and reconstruction can be an empowering part of that process.
At Breast Reconstruction Associates, our mission is to help women move forward with confidence through personalized, compassionate care. We specialize exclusively in breast reconstruction surgery, offering the latest techniques to help you achieve natural, long-lasting results.
The Power of Breast Reconstruction in Emotional Recovery
Breast reconstruction is more than a cosmetic procedure—it is a powerful step toward reclaiming your sense of self after breast cancer. Whether performed immediately following mastectomy or as a delayed reconstruction, the goal is to restore balance, femininity, and confidence.
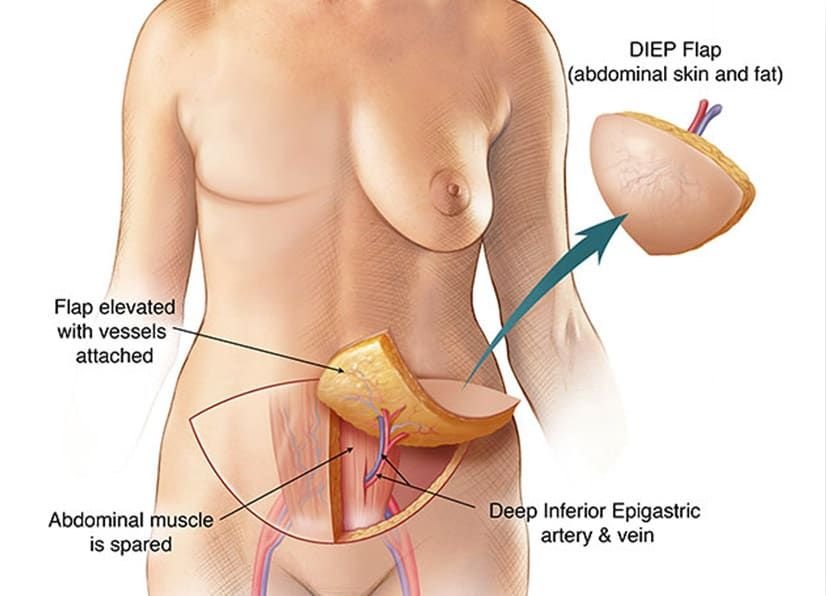
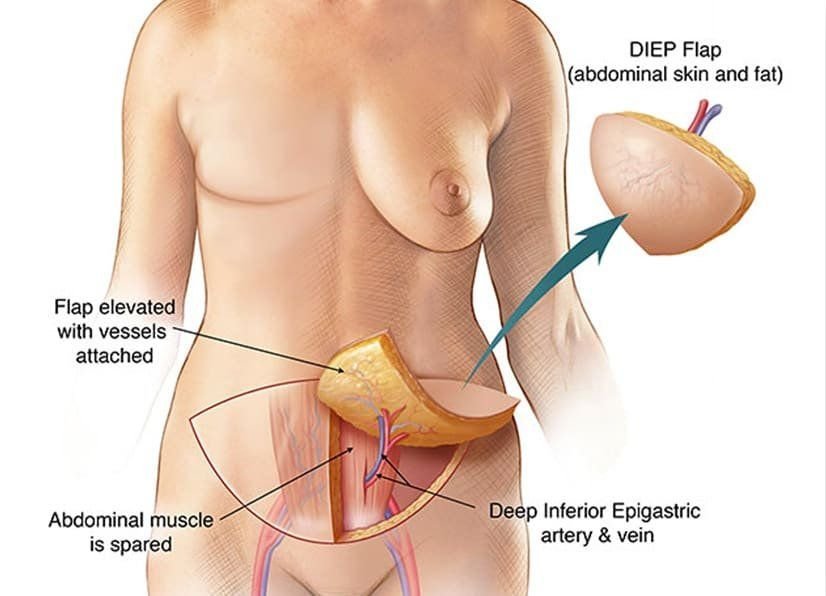
Our surgeons at Breast Reconstruction Associates are experts in microsurgical breast reconstruction, including the DIEP flap procedure—one of the most advanced and natural forms of breast reconstruction available today. This technique uses your own abdominal tissue to create a soft, natural breast while preserving abdominal muscles and core strength.
For women who are not candidates for DIEP flap surgery, we also offer other autologous reconstruction options such as the PAP flap and GAP flap, as well as implant-based reconstruction. Every treatment plan is customized to fit your medical needs, goals, and personal preferences.
Why Choose Breast Reconstruction Associates
At Breast Reconstruction Associates, you are more than a patient—you are family. Our board-certified surgeons combine advanced microsurgical expertise with genuine compassion and care. From your initial consultation to recovery, our team will walk beside you every step of the way.
We believe in education and empowerment. You will always receive honest, clear information about your options, so you can make the decision that feels right for you.
Our offices serve women throughout Texas and beyond, helping breast cancer survivors find strength, beauty, and confidence again.
A Season for Gratitude and Renewal
November is a time to honor resilience, healing, and gratitude. For many women, breast reconstruction represents more than recovery—it represents renewal and hope. Each journey is unique, and no matter where you are in yours, there is a path forward filled with compassion and possibility.
If you are exploring breast reconstruction in Texas, the caring team at Breast Reconstruction Associates is ready to help you understand your options and feel supported through every step.
Begin Your Healing Journey Today
You do not have to face this journey alone. Our specialists are here to help you rebuild with confidence and peace of mind.
Contact Breast Reconstruction Associates today at 682-200-8580 or visit txdiepflap.com to schedule your consultation.
Your healing begins with a conversation—and we are here to listen.