Love Yourself This February: Choosing Breast Reconstruction That’s Right for You
February is the month of love—a time to celebrate not just romantic relationships, but also the most important relationship of all: the one you have with yourself. For women who have faced the challenges of breast cancer, loving yourself often means embarking on a journey of healing and renewal. Breast reconstruction is a deeply personal choice that can help you feel whole and confident again.
At the Breast Reconstruction Associates, we believe every woman deserves to love the way she looks and feels. That’s why we specialize in DIEP flap breast reconstruction, a natural and long-lasting option that uses your body’s own tissue to create results that look and feel like you.
Why DIEP Flap Reconstruction?
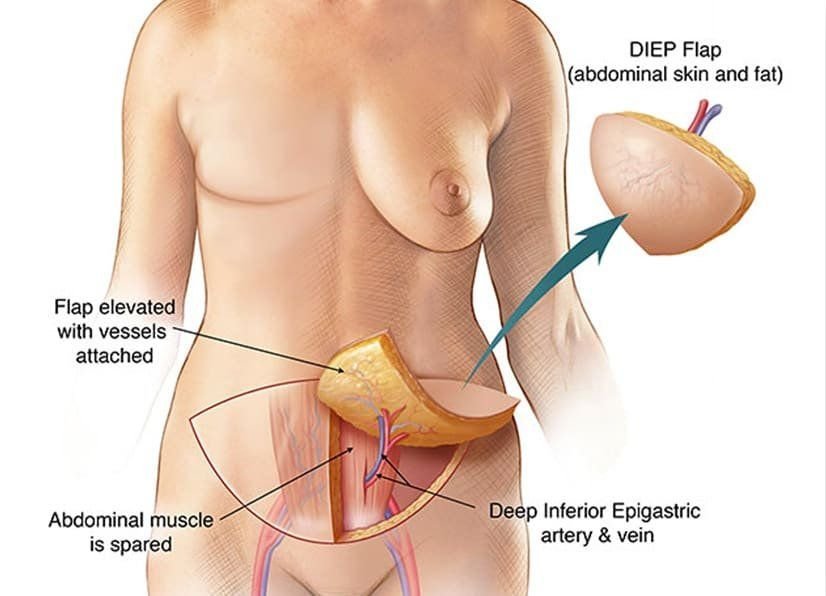
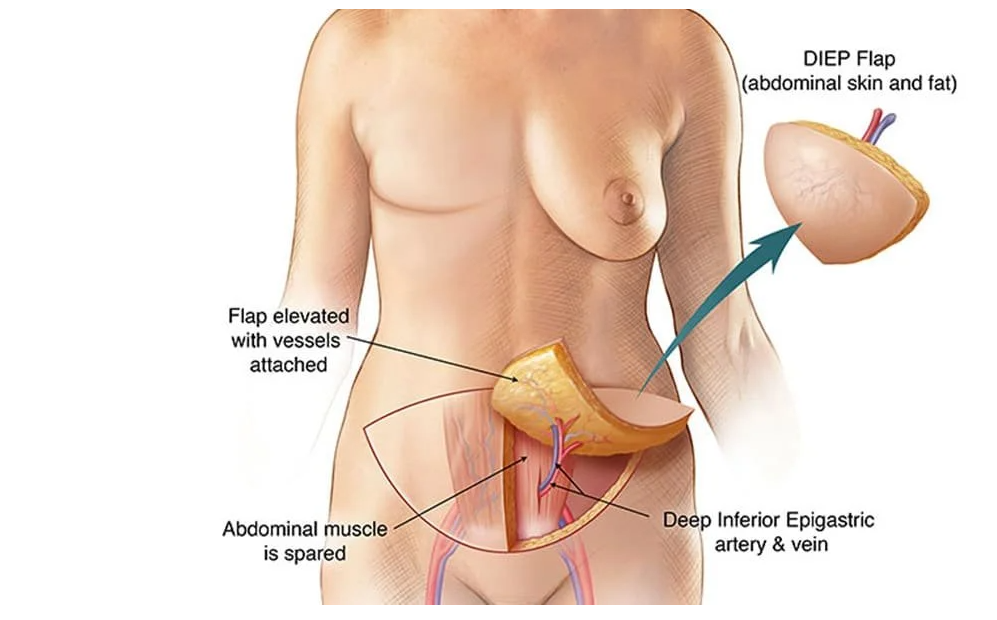
The DIEP flap procedure offers a unique set of benefits:
- Natural Results: Your own tissue is used, giving you a soft and natural appearance.
- Muscle-Sparing Technique: Unlike older methods, the DIEP flap doesn’t remove muscle, which helps reduce recovery time and preserve strength.
- Permanent Solution: With no implants, there’s no need for future replacements or adjustments.
By choosing DIEP flap reconstruction, you’re not just restoring your physical appearance—you’re also empowering yourself to embrace life after breast cancer with confidence.
Self-Love is Self-Care
Making the decision to undergo breast reconstruction is about more than just aesthetics; it’s about reclaiming your sense of self. Taking the time to care for your body and your well-being is a powerful act of self-love. Whether you’re newly diagnosed, in recovery, or years past your cancer journey, know that it’s never too late to prioritize yourself.
We’re Here to Help
This February, let us help you take the next step in your journey. Our team of highly trained microsurgeons is here to provide compassionate, personalized care tailored to your unique needs. Together, we’ll create a plan that restores not just your body, but also your confidence and sense of wholeness.
💖 Schedule a Consultation Today
📞 Call us at 682-200-8580
🌐 Visit us at txdiepflap.com
Because loving yourself starts with taking care of yourself. 💕