The Advantages of Having a Mastectomy
Breast cancer is one of the most common types of cancer among American women — nearly one in eight women develop it in the course of their lifetime. Treatment of breast cancer involves a multidisciplinary approach and therapies are selected based on biology, size, and location of the tumor. In most cases, surgical intervention is recommended, and patients are faced with the decision to undergo lumpectomy followed by radiation (known as breast conservation therapy) or mastectomy.
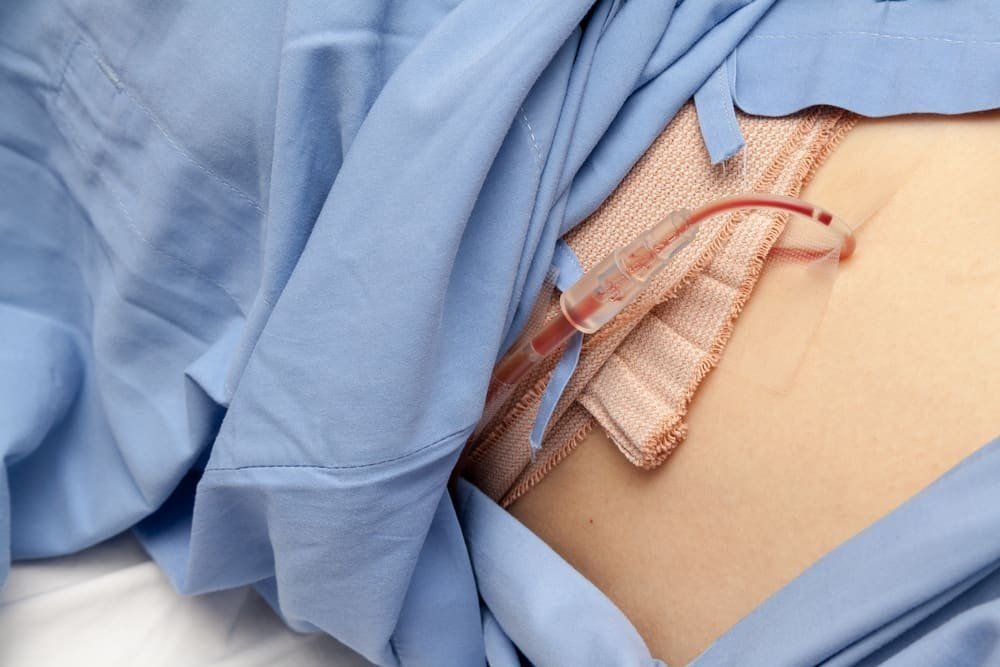
A mastectomy is the complete surgical removal of breast tissue. This surgical approach is appropriate for patients with breast cancer that does not meet the criteria for breast conservation therapy, patients who prefer mastectomy over BCT, or for prevention of breast cancer in high risk patients.
Historically, mastectomies included the removal of the overlying breast skin. Strategies to preserve the breast skin have now been developed that have significantly improved the cosmetic outcome of immediate breast reconstruction following a mastectomy. Patients who have a mastectomy followed by breast reconstruction can now have equivalent or superior cosmetic outcomes compared to breast conservation therapy.
There are other advantages of having a mastectomy over breast conservation. By choosing a mastectomy, patients have the potential to avoid the need for radiation therapy. This allows women to forgo the skin changes and other effects caused by radiation. Patients also no longer require regular mammograms following a mastectomy. And lastly, while research has demonstrated equivalent survival outcomes between mastectomy and breast conservation therapy, the risk of local recurrence is lower in patients who undergo mastectomy.
The decision to choose a mastectomy over other surgical treatment approaches is difficult and includes many variables. To determine the best plan for you, talk to your breast surgeon in Fort Worth.