Making the decision to undergo surgery, regardless of the
operation, can be overwhelming. At Breast Reconstruction Associates, we
understand that discussing the surgical details in plain English as well as
reviewing the potential risks involved imparts the needed information that
leaves patients feeling informed and confident.
A few of the general risks associated with any surgery are bleeding, infection of the surgical site, blood clots, and adverse reactions to general anesthesia. During your consultation with your plastic surgeon, you will review these general risks as well as the risks specific to breast surgery and/or reconstruction in detail. Although most women do not experience the following complications, here is a brief preview of the risks that will be covered in your discussion:
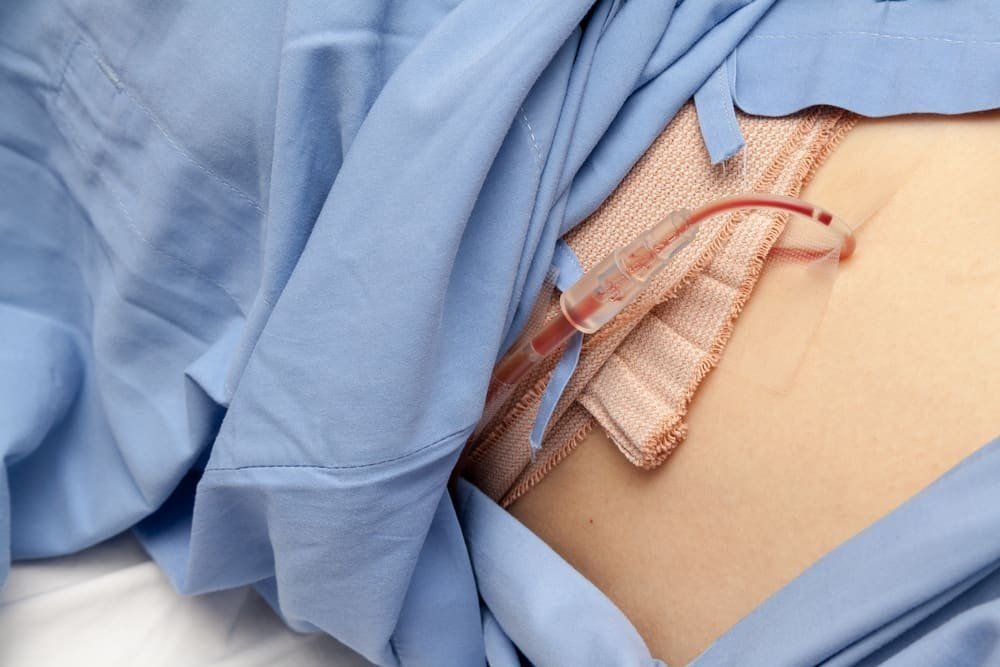
Fluid collections
Fluid or blood (seroma or hematoma) may accumulate between the skin and underlying tissues following surgery. Drains may be left in place after surgery to prevent this accumulation. Should this problem occur after drain removal, it may require additional procedures for drainage of the fluid.
Changes in sensation
The surgery will alter the sensation to the nipple, areola and surrounding breast skin. It’s important to discuss the possible extent of these changes with your surgeon, as it will depend on what type of surgery has been recommended for you.
Potential loss of the nipple-areola complex
If you are having a procedure that spares the nipple and areola, there is a risk of decreased vascular supply to these structures which can lead to necrosis (or death). This can either be self-limiting or require intervention.
Mastectomy flap necrosis
The breast skin remaining after mastectomy can have trouble healing from a lack of blood supply. When the blood supply is low enough, breast skin can die. This is more common in larger breasted women. Tobacco use and previous radiation history can also increase the risk of mastectomy flap necrosis.
Delayed wound healing
Wounds may separate after surgery. This may require daily home wound care or further surgery to correct the defect.
Microvascular thrombosis
Autologous breast reconstruction is associated with the risk of clot formation within the artery or vein providing circulation to the flap. This most commonly occurs during surgery but can happen afterwards, usually within the first 24-48 hours after surgery. This requires a second operation to attempt salvage of the tissue. The risk of this occurring is low and will be discussed in further detail with your surgeon.
Failure of the reconstruction –
Regardless of the method selected (implants, DIEP flap, or other flap), the reconstruction can fail which leaves the patient with a flat chest wall. Alternative methods would be considered if the patient elects to proceed with secondary reconstruction. In general, in properly selected patients, failure is uncommon.
At Breast Reconstruction Associates, we are committed to helping you navigate your surgical options, weigh the risks and benefits of surgery, and make the best decision specific to your care. Reach out to our plastic surgery office in Fort Worth, Austin or Oklahoma City if you have questions. We are here as a resource for you.